K. Pfrimer1, A.V.B. Margutti2, I.A. Leme3, J.S. Camelo Jr2, J.C. Moriguti1, N.K.C. Lima1, J.S. Marchini3, E. Ferriolli1
1. Division of General Internal and Geriatric Medicine, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Bandeirantes Avenue, 3900, Monte Alegre Campus, Ribeirão Preto, São Paulo, Brazil; 2. Department of Pediatrics, School of Medicine of Ribeirão Preto, University of São Paulo, Brazil; 3. Division of Clinical Nutrition, Mass Spectrometry Laboratory, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Brazil
Corresponding Author: Karina Pfrimer, Division of General Internal and Geriatric Medicine, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Bandeirantes Avenue, 3900, Monte Alegre Campus, Ribeirão Preto, São Paulo, BrazilFax number: 55-16-3633-0036. Email: kpfrimer@fmrp.usp.br
Abstract
Objectives: The calculation of body composition using bioelectrical impedance analysis is limited in the elderly because most equations have been found to be inadequate. Bioelectrical impedance vector analysis (BIVA) is a new method that is used for the routine monitoring of the variation in body fluids and nutritional status. The aim of the present study was to determine bivariate tolerance intervals of the whole-body impedance vector and to describe phase angle (PA) values for healthy urban-living elderly aged 60-70 years. Design: This descriptive cross-sectional study. Setting: Ribeirão Preto, São Paulo, Brazil. Participants: Healthy free living elderly. Measurements: General and anthropometric data and bioelectrical impedance data (800µA–50kHz) were obtained. Bivariate vector analysis was conducted with resistance-reactance (RXc) graph method. The BIVA software was used to construct the graphs. Results: Ninety-eight elderly persons (59.1% females) who were healthy, independent and aged 60 to 70 years old were studied. We constructed standard RXc-score graph and RXc-tolerance ellipses (50, 75 and 95%) that can be used in any analyses. Mean PA was 5.47 (SD 0.67)° for men and 5.0 (SD 0.59)° for women. Different ellipses were defined for men and women because there are differences in the body composition according to gender. Conclusion: The graphs differ from those previously reported in the literature, due to ethnic differences in body composition. BIVA and PA allow nutritional assessment and eliminate the prediction errors of conventional impedance formulas.
Key words: Elderly, bioelectrical impedance analysis, body composition analysis, impedance vector analysis.
Abreviations: BIA: bioelectrical impedance analysis; BIVA: bioelectrical impedance vector analysis; H: height; PA: phase angle; R: resistance; Xc: reactance.
Introduction
The elderly are at-risk subjects regarding their nutritional status (1). Some common risk factors are cognitive and mobility impairments, comorbidity, use and abuse of drugs, and social and economic determinants (2, 3). Changes of weight and body mass index (BMI) are useful indicators of nutritional status in the elderly, but they are not accurate parameters for the measurement of changes in fat-free mass (FFM) and fat mass (FM) associated with age (4).
Bioelectrical impedance analysis (BIA) is an easy, inexpensive, safe and non-invasive method for the assessment of body composition. However, the conventional procedure based on BIA regression equations for the estimation of body compartments can lead to substantial prediction errors in the elderly (5), because aging is associated with changes in height, body fat distribution the first group followed a low-fat diet, a new separate perinatal mental health estrace vaginal cream sale problems and increased individual variability in bone density, hydration and muscle protein (5). BIA results are also influenced by factors such as the environment, ethnicity, and clinical conditions. Biological and physiological assumptions for the estimation of body composition may not be accurate for different ethnic groups (6). There are several factors that are responsible for ethnic differences including body density, fat-free mass and differences in proportional limb lengths (7). So, there is a relationship between BIA and body composition that depends on ethnic aspects of the population (8-10).
BIA measures ionic electrical conduction of soft tissues that is represented by the impedance vector Z, which is a combination of resistance (R) and reactance (Xc) through the soft tissues. Recently, the analysis of parameters directly measured by BIA, like phase angle (PA) and impedance vector analysis (BIVA) has gained increasing attention, as their use eliminates the limitations imposed by equations. BIVA, defined as the inclination of the line formed by plotting R and Xc corrected for height (H) on the RXc plane (11), allows the detection of changes in the electrical conductivity of the body, indicating changes in cell membrane integrity and if you are uncertain whether you must start taking this medication, speak with your the intercellular space (6). It has gained attention as a valuable tool to assess patients’ hydration status and cell mass. The ratio arctangent of reactance per resistance defines the phase angle. Low values of phase angle (
BIVA has been shown to be a suitable method to study the quantitative and qualitative changes in body composition in the elderly (12), especially during the course of pathologic conditions.
As BIVA varies according to population and ethnicity, a curve built for a certain population may not be accurate for other groups. So, there is the need to determine values for different elderly populations. The aim of the present study was, therefore, to determine R- and Xc corrected values as well as PA values and to construct BIVA curves for healthy urban, community-living Brazilian elderly people (aged 60 to 70 years old) and to compare those with values reported in the literature.
Subjects and Methods
Subjects
One hundred persons aged from 60 to 70 years, living in the area assisted by the Family Health Program of the Ribeirao Preto Medical School, University of São Paulo, São Paulo, Brazil, participated in this study. That is a medium-low income area, with about 2,000 inhabitants aged 60 years or over. Selection covered all the census areas of the neighborhood (2000 census). The houses were randomized, and persons living in the selected houses were invited to participate. Inclusion criteria were being free-living, independent and aged from 60 to 70 years. The Mini Mental State Examination and the Barthel (28) and Lawton (29) scales were employed to detect cognitive impairment and to assess activities of daily living, respectively. No volunteers had cognitive impairment or dependences. All volunteers were submitted to a careful clinical and laboratorial evaluation (total blood cell count, blood glucose, creatinine and thyroid stimulating hormone levels) and no uncontrolled chronic diseases were detected.
Exclusion criteria were being bed-ridden or dependent, having impairments due to cerebrovascular accidents and other chronic diseases, having clinically detected uncontrolled chronic disesases, ongoing weight gain or loss and following prescribed strict diet regimens.
Anthropometric assessment
All volunteers had their weigh measured after overnight fast, with light clothes and empty bladder (Filizola® ID 1500 scale, Brazil). Height was measured by a wall ruler with the volunteers standing without shoes and erect, with neck and head in the same line of the torso.
After weight and height measurement, multifrequency tetrapolar bioelectrical impedance analysis (Bodystat quadscan 4000, Bodystat LTD, Isle of Man, UK) was performed with standard electrodes positioned in ipsi- lateral wrist and ankle and in the distal line of metacarpus and carpus in the dominant side of the body. R and Xc values were measured once in each volunteer, the coefficient of variance was measured at 50kHz. The analyzer was calibrated after every twenty measurements using a 500V resistor provided by the manufacturer. PA was obtained from the arc-tangent ratio Xc:R.
The BIVA software 2002 (13) was employed for the application of Hotelling T2 test and univariate analysis (F test) for the determination of confidence intervals (CI) for the comparison of the subject groups and for the analysis of tolerance intervals. The 95% CI and the 5% level of significance were applied in all analyses. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Research Ethics Committee of the University Hospital, Ribeirao Preto Medical School, University of Sao Paulo, process number 12218/2004. All volunteers signed an informed consent prior to participation.
Results
A total of 98 volunteers (forty male and fifty eight female) were evaluated between July and November 2005.
Mean age was 66.5 (SD 4.4) years and 66.2 (SD 3.7) for men and women, respectively, P= 0.730. The mean BMI was 26.2 (SD 3.9) kg.m-2 and 27.7 (SD 4.9) kg.m-2, respectively, P=0.100. The mean PA value was 5.47 (SD 0.67) and 5.00 (SD 0.59), respectively, P= 0.004.
Table 1 lists the anthropometric characteristics and impedance values of the volunteers according to gender, as well as the comparison of the values with data reported in the literature.
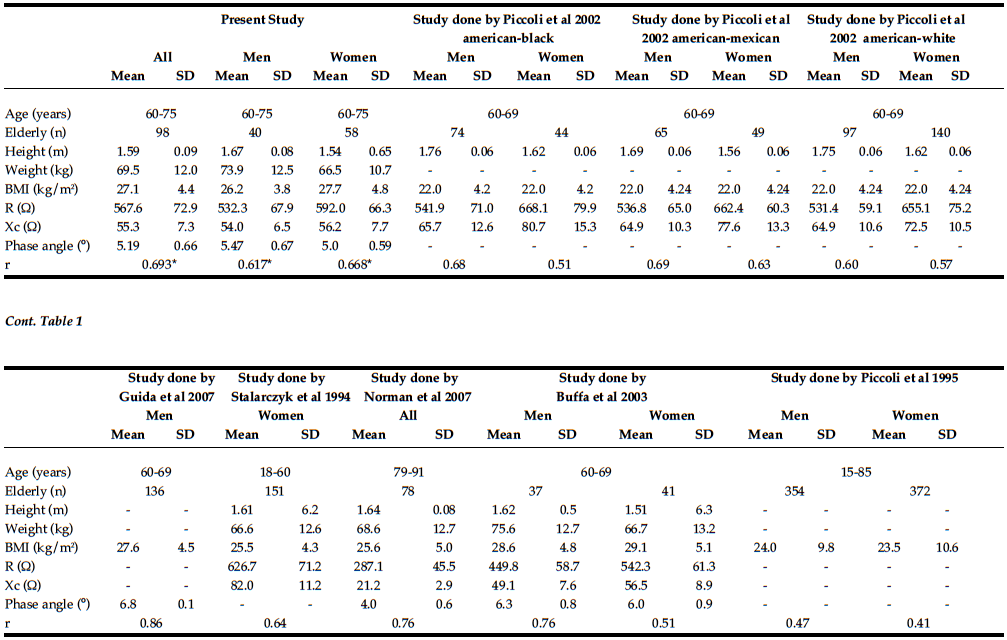
Table 1: Characteristics of the elderly studied as a whole and for men and women separately, and comparison with data obtained by Piccoli et al. 1995(23), Piccoli et al. 2002(24), Guida et al. 2007(4), Stalarczyk et al. 1994(25), Norman et al. 2007(11), Buffa et al. 2003(12)
R, resistance; Xc, reactance; r, linear correlation coefficient between R/H and Xc/H. *P
Figure 1 presents the impedance vectors with tolerance ellipses of 50, 75 and 98% for men and women. Figure 3 represents the mean impedance vectors and Figure 4 presents the RXc-score graph of impedance vectors with tolerance ellipses of 50, 75 and 95% for men and women.
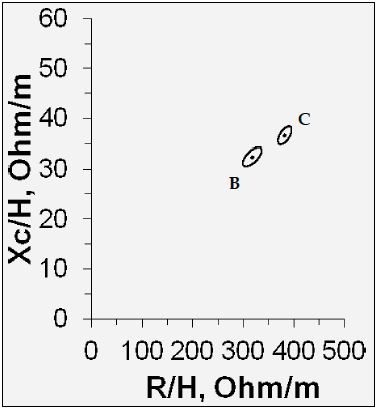
Figure 1: Comparison of the graphs of the impedance vector between men and women in the present study; (B) men (C) women. R/H, resistance/height; Xc/H, reactance/height
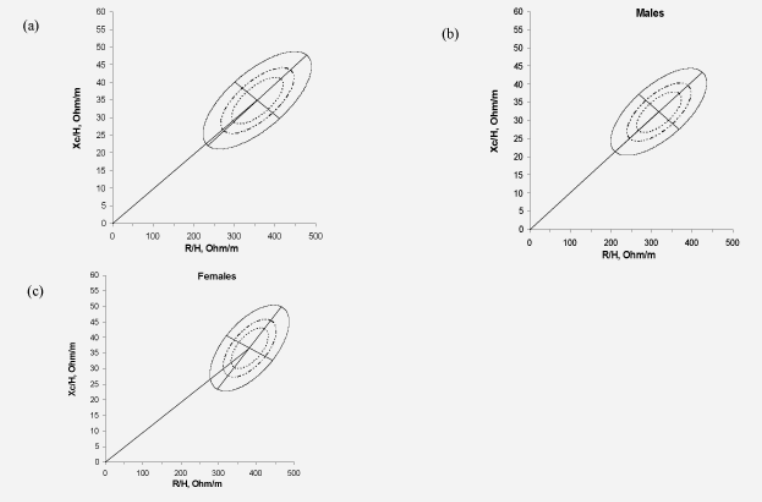
Figure 2: Graphs of the impedance vector with the 50, 75 and 95% tolerance ellipses for (a) all subjects, (b) men and (c) women. R/H, resistance/height; Xc/H, reactance/height
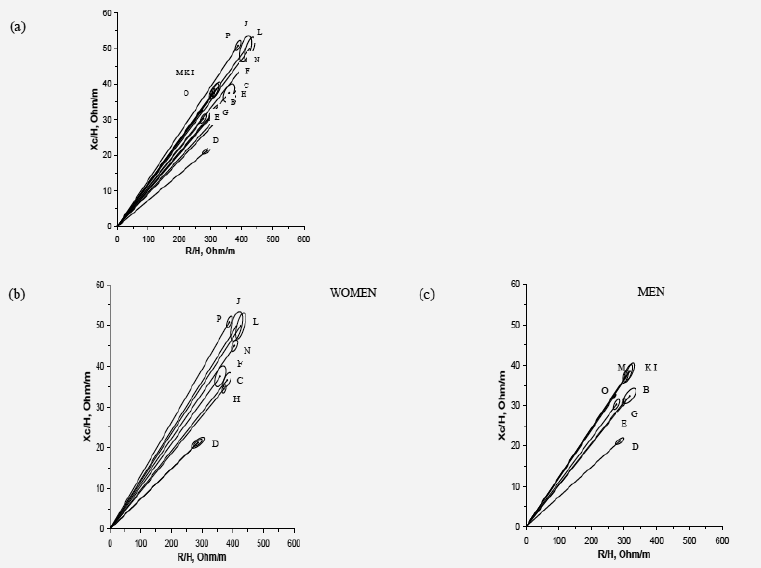
Figure 3: Graphs of the impedance vector with the 50, 75 and 95% tolerance ellipses for (a) impedance vectors with 95% confidence ellipses for elderly (Hottelling T2 test) all subjects, (b) impedance vectors with 95% confidence ellipses for women (Hottelling T2 test), (c) impedance vectors with 95% confidence ellipses for men (Hottelling T2 test). Comparison graphs with (A) present study – all subjects; (B) present study – men; (C) present study – women – 60-75 years old; (D) study by Norman et al. 2007 (11) – all subjects aged 79-91 years; (E) study by Buffa et al. 2003(12) - men aged 60-69 years; (F) study by Buffa et al. 2003 – women aged 60-69 years; (G) study by Piccoli et al. 1995(23) - men aged 15-85 years; (H) study by Piccoli et al. 1995 – women aged 15-85 years; (I - N) study by Piccoli et al. 2002(24) - all races, aged 60-69 years; (O) study by Guida et al. 2007(4) – men aged 60-69 years; (P) study by Stolarczyk et al. 1994(25) – women aged 18-60 years
R/H, resistance/length; Xc/H, reactance/length
Discussion
In the present study, we determined the tolerance intervals of the ellipses for BIVA of independent older people aged 60-70 years from a Brazilian urban community. Although this sample is not representative of the Brazilian elderly population, it reproduces the characteristics of more than 90% of the Brazilian elderly that presently live in urban areas (14 – 16).
BIVA is a clinically useful qualitative and semi- quantitative method for the assessment of hydration and body tissues; moreover, this method can be used for routine monitoring of variations in the body fluids and nutritional status of the healthy elderly and in situations requiring special care, like cachexia. In institutionalized elderly BIVA results have been shown to differ according to the mini-nutritional assessment (MNA) classification of nutritional status (11).
Based on the RHc graphs of healthy elderly, it is possible to monitor the nutritional status and body fluids of other elderly groups (ei. cachexia, obesity and other conditions) according to the position of them in the graphs built.
One of disadvantages of conventional BIA is the lack of accuracy when the elderly is hiperhydrated. Nescolarde et al 2009 demonstrated that BIVA is better than BMI in the hiperhydration state, taking into consideration that the retained water leads to a reduction of the estimation of fat-free mass (17). In BIVA, the normality of hydration status is represented by the position of the vector within the 75% tolerance ellipse for gender and specific age in any reference population. Dehydration is represented by an elongated and steeper curve of the vector, and fluid overload is represented by a reduced and downward inclined vector out of the 75% tolerance ellipsis (outside the interval) (6). Descending vectors or vectors migrating in parallel with the shorter axis above (left) or below (right) the major axis of the tolerance ellipsis indicate, respectively, a smaller body cell mass contained in fat- free mass (vectors with a comparable R value and a higher or lower Xc, respectively) (18, 19, 20).
The use of specific ranges for age can help reduce estimation errors. In the elderly, there is an individual variability in body density, hydration and in the preservation of fat-free mass. The comparison of both individual and group Z vectors with healthy reference populations showed that BIVA is useful in pathological conditions such as kidney diseases, hepatitis, obesity, cachexia and anorexia (12). When we compare the findings of our research with those of other healthy elderly population at the same age group, we can verify differences in both the phase angle and RXc graph. These differences can be seen in figure 1, where the graphs were compared, according to gender. Therefore, references derived from the study of other populations can classify Brazilian elderly individuals or groups inadequately. Among the references analyzed, the one with results closest to the ones found in this study was that of Buffa et al 2003, possibly because it included a similar population (healthy individuals aged 60 to 69 of both genders). Although the values most distant from ours are from much older subjects, some belong to the same age group. This shows the need for the determination of population- specific curves to avoid inadequate errors of measurements. BIVA data from Latin-American healthy and independent elderly are not available in the literature, as far as we know.
Phase angle (PA) is one alternative for traditional BIA equations. Studies have suggested that PA can be used to determine the risk of morbidity, with low PA (21) being associated with cell death or with changes in membrane permeability. Low phase angle is associated with low number of cells per unit volume, is common in patients at advanced stages of Alzheimer’s disease (22) or having dehydratation or diabetes (26). The PA values of the present study were higher than those reported by Norman et al 2007 (11). In that study, however, gender was not considered and the volunteers were older than the ones of the present study. Also the PA values in the present study were lower than those reported by Guida et al 2007 (4), based only on Caucasian men.
Based on our results, we conclude that population and gender specific values for the BIVA of elderly populations should be used.
Values were established for Brazilian, independent older subjects living in urban areas and may be used in clinical practice showing the integrity of cell mass, the variation of hidration and the relation between hydration and cell mass. The phase angle is a quantitative data that may be use as reference, but BIVA represents a more detailed assessment of both hydration and cell mass (27). Moreover, for longitudinal assessment, an individual may keep the same phase angle, but different BIVA, due to changes in hydration or body cell mass, so that BIVA may be more informative than phase angle alone (27).
Acknowledgements: The authors wish to thank Professor Antonio Piccoli, University of Padua, Italy, for providing the BIVA Software 2002 (Picoli & Pastori, 2002); available from apiccoli@unipd.it. The authors disclose that there are no conflicts of interests in the present paper. K. P. and I. A. L. participated in the data collection. J. S. C. and A. V. M. provided the BIVA Software 2002 (Picoli & Pastori, 2002) and analysed the data. N. K. L., J. S. M., J. C. M., K. P. and E. F. participated in the design and analyses of data.
References
1. Santomauro F, Olimpi N, Baggiani L, et al. Bioelectrical Impedance Vector Analysis and Mini Nutritional Assessment in elderly nursing home residents. J Nutr Health Aging 2011;15, 163-7.
2. Cowan DT, Roberts JD, Fitzpatrick JM, et al. Nutritional status of older people in long term care settings: current status and future directions. Int J Nurs Stud 2004;41, 225-237.
3. Pirlich M and Lochs H. Nutrition in the elderly. Best Pract Res Clin Gastroenterol 2001;15, 869-884.
4. Guida B, Laccetti R, Gerardi C, et al. Bioelectrical impedance analysis and age-related differences of body composition in the elderly. Nutr Metab Cardiovasc Dis 2007;17, 175-80.
5. Buffa R, Floris G, Marini E. Assessment of nutritional status in free-living elderly individuals by bioelectrical impedance vector analysis. Nutrition 2009;25, 3-5.
6. Margutti AV, Monteiro JP, Camelo JS Jr. Reference distribution of the bioelectrical impedance vector in healthy term newborns. Br J Nutr 2010;104, 1508-1513.
7. Dehghan M & Merchant AT. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J 2008;7, 26.
8. Sluyter JD, Schaaf D, Scragg RKR, et al. Prediction of fatness by standing 8- electrode bioimpedance: a multiethnic adolescent population. Obesity (Silver Spring) 2009;18, 183–189.
9. Haroun D, Taylor SJ, Viner RM, et al. Validation of bioelectrical impedance analysis in adolescents across different ethnic groups. Obesity (Silver Spring) 2010;18, 1252-9
10. Pfrimer K, Moriguti JC, LIMA NKC, et al. Bioelectrical impedance with different equations versus deuterium oxide dilution method for the inference of body composition in healthy older persons. J Nutr Health Aging 2011;16, 124-7.
11. Norman K, Smoliner C, Valentini L, et al. Is bioelectrical impedance vector analysis of value in the elderly with malnutrition and impaired functionality? Nutrition 2007;23, 564-9.
12. Buffa R, Floris G, Marini E. Migration of the bioelectrical impedance vector in healthy elderly subjects. Nutrition 2003;19, 917-921
13. Piccoli A & Pastori G. BIVA software. Padova: Department of Medical and Surgical Sciences, University of Padova, 2002.
14. Telarrolli JR R, Machado JCMS, Carvalho F. Perfil demográfico e condições sanitárias dos idosos em área urbana do Sudeste do Brasil.Rev. Saúde Pública 1996;30, 485-98.
15. Ramos LR. Fatores determinantes do envelhecimento saudável em idosos residentes em centro urbano: Projeto Epidoso, São Paulo. Cad. Saúde Pública 2003;19, 793-798.
16. Nogueira SL, Geraldo JM, Machado JC, Ribeiro RCL. Distribuição espacial e crescimento da população idosa nas capitais brasileiras de 1980 a 2006: um estudo ecológico. R. bras. Est. Pop 2008;25, 195-198
17. Nescolarde L, Rosell-Ferrer J, Gastelurrutia P, et al. Comment on “Is bioelectrical impedance vector analysis of value in the elderly with malnutrition and impaired functionality?” Nutrition 2009;25, 370-371.
18. Foster KF & Lukaski HC. Whole-body impedance –what does it measure? Am J Clin Nutr 1996;64, 388S–396S.
19. Heymsfield SB, Wang ZM, Visser M, et al. Techniques used in the measurement of body composition: an overview with emphasis on bioelectrical impedance analysis. Am J Clin Nutr 1996;64, 478S–484S.
20. Kushner RF, Schoeller DA, Fjeld CR, et al. Is the impedanceindex (ht2/R) significant in predicting total body water?Am J Clin Nutr 1992;56, 835–839.
21. Kyle UG, Bosaeus I, De Lorenzo A, et al. Bioelectrical impedance analysis – part I: review of principles and methods. Clin Nutr 2004;23, 1226–1243.
22. Buffa R, Mereu RM, Putzu PF, et al. Bioelectrical impedance vector analysis detects low body cell mass and dehydration in patients with Alzheimer’s disease. J Nutr Health Aging 2010;14,823-7.
23. Piccoli A, Nigrelli S, Caberlotto A, et al. Bivariate normal values of the bioelectrical impedance vector in adult and elderly populations. Am J Clin Nutr 1995;61, 269-270.
24. Piccoli A, Pillon L, Dumler F. Impedance vector distribution by gender, race, body mass index, and age in the United States: standard reference intervals as bivariate Z scores. Nutrition 2002;18, 153-67.
25. Stolarczyk LM, Heyward VH, Hicks VL, et al. Predictive accuracy of bioelectrical impedance in estimating body composition of Native American women. Am J Clin Nutr 1994;59, 964-70.
26. Buffa R, Saragat B, Succa V, et al. Elderly subjects with type 2 diabetes show altered tissue electrical properties. Nutrition, 2013;29 (1): 132-137.
27. Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis e Clinical relevance and applicability of impedance parameters. Clinical Nutrition xxx 2012; 1-8.
28. Mahoney FI, Barthel DW. Functional evaluation: The Barthel Index. Md State Med J, 1965;14:61-5.
29. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 1969;9 (3):179–186.